The Philippine Acceleration Action Plan for Tuberculosis (PAAP-TB) 2023-2035 aims to achieve TB elimination in the Philippines by integrating TB elimination commitments into the mandates, policies, and work programs of government agencies represented in the TB National Coordinating Committee (NCC).


The Philippine Acceleration Action Plan for Tuberculosis (PAAP-TB) 2023-2035 aims to achieve TB elimination in the Philippines by integrating TB elimination commitments into the mandates, policies, and work programs of government agencies represented in the TB National Coordinating Committee (NCC).
The PAAP-TB focuses on addressing the social determinants of health, ensuring equitable access to care, and actively detecting TB cases through a multi-sectoral approach. It promotes health-risk reduction behaviors and increases demand for TB protection and care to improve the health and well-being of all Filipinos.
Tuberculosis (TB) remains a critical public health issue in the Philippines that requires a holistic approach to tackle social determinants of health and ensure equitable access to care. Despite global efforts to eliminate TB, the current response is inadequate and disparities persist in service access.
The high incidence of TB also exacerbates poverty by making it difficult for those affected to work due to illness and associated stigma.









Tuberculosis (TB) remains a critical public health issue in the Philippines that requires a holistic approach to tackle social determinants of health and ensure equitable access to care. Despite global efforts to eliminate TB, the current response is inadequate and disparities persist in service access. The high incidence of TB also exacerbates poverty by making it difficult for those affected to work due to illness and associated stigma.




To effectively reduce TB transmission, improve access to quality TB services, and lower disease incidence, addressing social, economic, and physical determinants is crucial. These factors influence up to 70% of health outcomes and require a comprehensive approach to reduce disparities and promote health equity. The Department of Health’s 2023-2028 Health Sector Strategy recognizes the critical importance of addressing social determinants of health and prioritizes their impact on population health.
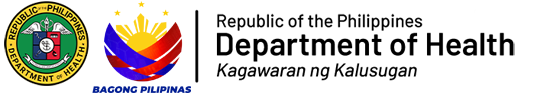
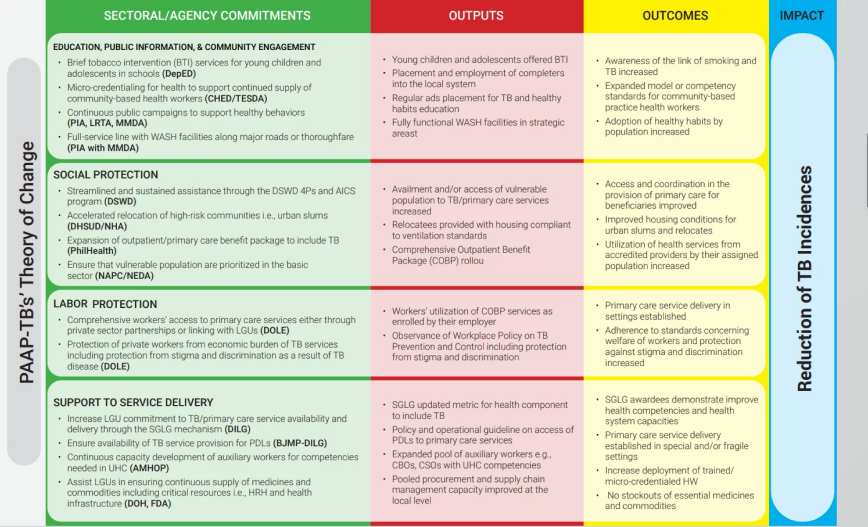
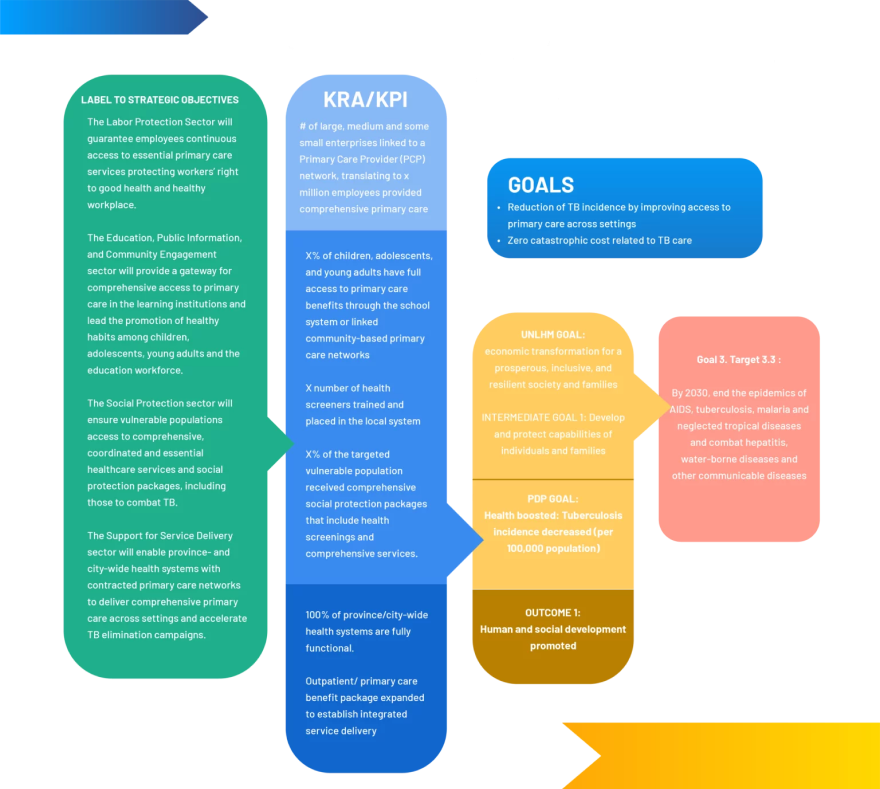
The DOH’s Disease Prevention and Control Bureau (DPCB) seeks to enhance the Philippine Strategic TB Elimination Plan (PhilSTEP) into a comprehensive, multisectoral initiative through the Philippine Acceleration Action Plan for Tuberculosis (PAAP-TB) (see Figure 1). With the PAAP-TB as its framework, the DPCB aims to coordinate efforts across multiple sectors beyond 2023 to make significant progress towards tuberculosis elimination in the Philippines. The PAAP-TB serves as the cornerstone for the TB National Coordinating Committee’s (TB-NCC) member agencies to align their TB elimination efforts with their organizational plans, policies, and programs. The objective is to encourage healthy behaviors and elevate demand for TB protection and care. The PAAP-TB acts as a central platform for addressing various determinants of health, and to enhance collaboration among stakeholders by sharing information and best practices.
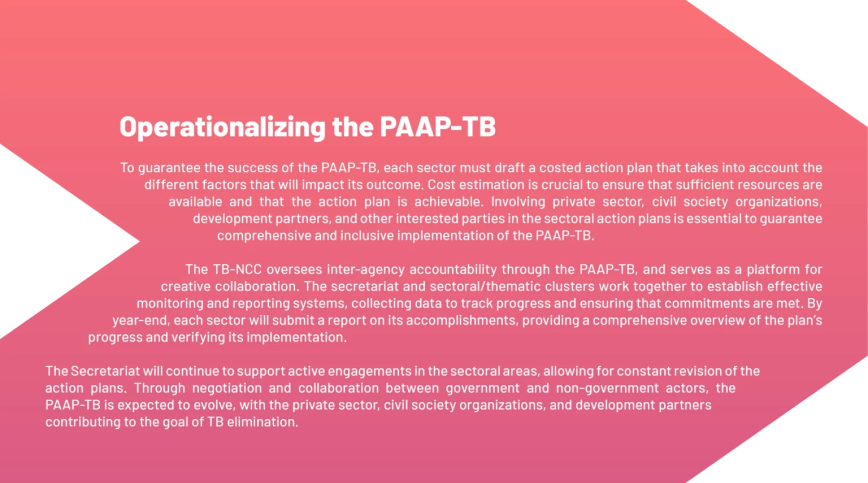
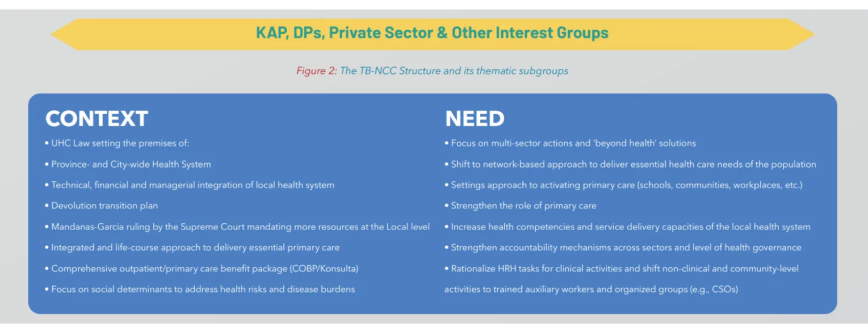
To this end, subgroups have been established (see Figure 2) to address specific Social Determinants of Health (SDH), and core members provide guidance and play a leadership role. These subgroups, also known as sectoral/action areas, are responsible for fostering collaboration between the TB-NCC and stakeholders, exchanging information related to their focus areas, an executing their respective tasks within the PAAP-TB framework, all with the aim of promoting health equity and reducing disparities in TB incidence.
The key to successfully eliminating tuberculosis lies in collaboration and participation from all relevant parties. The TB-NCC plays a vital role in this effort, while also encouraging active engagement from key affected populations and stakeholders to make meaningful contributions towards controlling and eliminating tuberculosis in the Philippines (see Figure 3).a
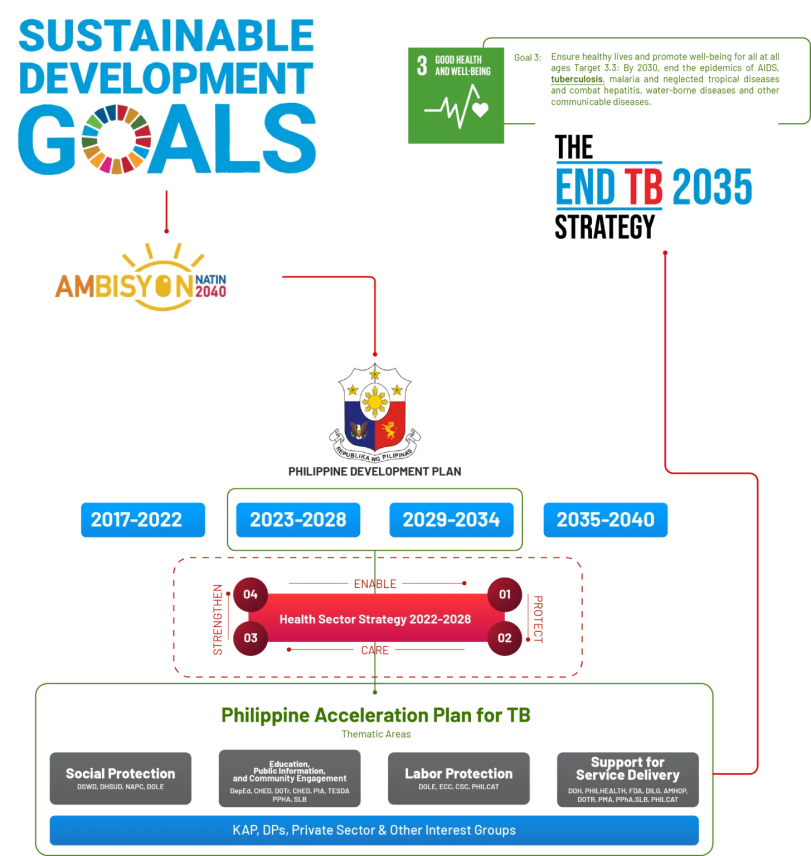
To improve collaboration and support among involved organizations and partners, the TB-NCC will be strengthened as a collegial platform. The TB-NCC will facilitate the exchange and sharing of data, ensuring accountability for assigned roles and responsibilities. Instead of working in isolation, the TB-NCC will become a space for coordinating and enhancing the core mandate and strengths of each member.
To achieve the desired health outcomes, PAAP-TB prioritizes TB over other pressing health issues. As part of this effort, the TB-NCC will launch a joint advocacy campaign aimed at broadening the scope of how TB disease burden is addressed. Active collaboration across the envisioned revitalized multisector platform of the TB-NCC will be essential in supporting the country’s efforts to eliminate TB. The expected benefits of this collaboration include the TB-NCC becoming more boundary-spanning, outcomes-focused, enabling, and effective in preventing TB.
However, achieving all of these goals will depend on how effectively the TB-NCC assists stakeholder agencies in maximizing and utilizing their competencies. This includes setting clear objectives aligned with their existing purpose and structure, engaging with strong political commitment, setting up viable organizing structures, building a culture of collaboration and ownership, providing incentives for partnership within their agencies’ scope, managing networks and gaps, and launching effective and sustainable social and behavior change communication (SBCC) interventions through advocacy campaigns.
To succeed, the IRR of RA10767 requires various functions, such as coordination, technical support, monitoring, and evaluation. The PAAP has two medium-term goals, which will need to be reviewed and adjusted as needed by the current administration. A multi stakeholder approach is necessary for success, with sectoral representatives and organizations working together through clusters. The DOH must fully support the TB-NCC agencies’ involvement in PAAP processes and activities, and stakeholders need capacity building and technical assistance. Operational policies and a strategic communication plan are crucial for effective implementation and coordination of actions among agencies.
Core members will have decision-making authority and roles, and each thematic area will be led by a core member. As deliberations may require interagency collaboration or convergent actions, representatives should be able to answer for and decide on behalf of their agency in this high-level governing body.
Therefore, the representative designated to the committee should be at the level of Undersecretary or their equivalent for each agency, as a permanent representative, with a designated alternate within the Executive Board or decision-making body/committee, i.e., Assistant Secretary.
Full committee meetings should have a more strategic agenda rather than an operational one, leaving the latter to be handled by an implementation arm. This ensures that the committee focuses on key decision-making processes while enabling an implementation arm to handle operational matters.
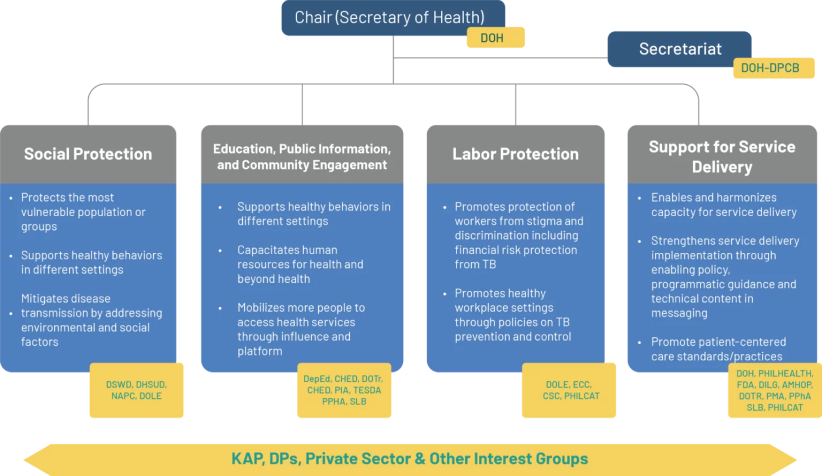
The core members were selected based on the scope and reach of each agency’s mandate in advancing and addressing SDH. The DOH serves as the committee’s secretariat and streamlines all health initiatives. Core members will address intersectoral and cross-cutting issues, including those requiring decisions on the committee’s ways of working and convergent actions at the national and local levels.
Thematic clusters and expanded membership have been organized to address variations in relevant SDH and facilitate a more concerted effort involving other stakeholder agencies and organizations. Subgroups will increase the likelihood of achieving concrete results by encouraging the exchange of information, experience, and best practices.
Core members will coordinate the work within each thematic area and lead each subgroup.
- The social protection subgroup will be led by DSWD and composed of NEDA, DOTR, DSHUD, and DOLE.
- The Education, Public Information, and Community Engagement cluster will be led by DepEd and CHED, with TESDA and PIA as members.
- The Support for Service Delivery and Implementation subgroup will be led by DILG, DOH, and ULAP.
- The Labor Protection Stakeholders subgroup will engage the private sector based on their needs and shared interests.
- To cascade decisions from the national level to the regional and local levels, the Regional Coordinating Committee (RCC) or other multi-sectoral collaborating committees located in the provinces or highly-urbanized cities (HUCs) and municipalities shall be included in the TB-NCC structure. The RCC will coordinate implementation at the subnational level and ensure close collaboration with targeted LGUs.
Before being implemented nationwide, the RCC’s suggested roles could be initially scoped at a specific locus, including coordinating and driving implementation across different sectors at the sub-national level based on commitments, ensuring focused work with targeted LGUs, and implementing, executing, and monitoring & evaluating. The unit is proposed to be lodged under the Regional Social Development Committee (RSDC), which is a subcommittee of the Regional Development Council (RDC) and is the highest policy-making body in each region.
DOH’s Disease Prevention and Control Bureau (DPCB) or its equivalent will serve as the technical secretariat’s head, assisted by a selected unit and/or as appointed by the Secretary of Health, who will be responsible for TB-related initiatives.
Depending on circumstances or needs, the Chair may call upon other divisional staff members and units to join the Technical Secretariat.
In general, the key functions of the Secretariat shall include:
1. Driving core agency mandates by clarifying operational policy and plans so the NCC remains accountable in steering, decision-making, and actions enacted by member agencies.
2. Ensuring NCC members fulfill and deliver commitments, such that accountabilities remain monitored.
3. Identifying and bridging policy gaps using dialogues or bilateral discussions to ensure social protection programs and specific interventions can serve the sectors unreached by the system;
4. Addressing gaps between policy and execution, especially where more effective TB NCC and RDC links need to be studied and rationalized




1. What is the TB-NCC and its role?
The Comprehensive Tuberculosis Elimination Plan Act of 2016 (RA 10767) creates the TB National Coordinating Committee (TB-NCC) in the Philippines to promote a collaborative, government-wide approach to eliminating TB. The TB-NCC actsas a high-level steering committee, promoting accountability and coordination among agencies and sectors. To achieve its goals, the TB-NCC must operate with transparency, trust, accountability, communication, and efficient resource management.
2. What are social determinants of health and how do they TB?
Social determinants of health are the social and economic factors that influence an individual’s health and well-being, including poverty, education, housing, and employment. These conditions can greatly impact the occurrence and transmission of tuberculosis, as poverty, overcrowding, malnutrition, lack of healthcare, poor sanitation, and low education levels can all weaken immunity and increase susceptibility to TB. Addressing social determinants of health is essential for reducing TB incidence and improving health outcomes for affected populations.
3. Why is there a need to address the social determinants of TB?
TB remains a significant burden, requiring a comprehensive approach that addresses social determinants of health and ensures equitable access to care. The global response to TB is inadequate, with disparities in diagnosis and treatment success due to lack of comprehensive interventions. Addressing social, economic, and physical barriers is necessary to improve access to TB care and reduce disease incidence.
The Philippines continues to face chronic poverty and poor health outcomes, particularly among the lowest income group. Addressing TB through a strategy informed by social determinants is critical for reducing health disparities and promoting health equity. Improving access to quality primary care and proactive clinical interventions is key.
To reduce the TB burden, strategies must address social determinants, which can account for up to 70% of health outcomes. The Department of Health’s 2023-2028 Health Sector Strategy prioritizes social determinants of health, recognizing their significant impact on the population’s health.
4. What is PAAP-TB?
The DOH Disease Prevention and Control Bureau (DPCB) and its partners developed the Philippine Strategic TB Elimination Plan (PhilSTEP) in 2018 to support the global effort to end TB. DOH DPCB aims to reconfigure PhilSTEP into a multisectoral plan after 2023. The USAID’s TB Innovations, Health Systems Strengthening (TB IHSS) Project supports this reconfigured strategy through the Philippine Acceleration Action Plan for Tuberculosis (PAAP-TB).
PAAP-TB serves as the basis for NCC agencies to integrate their TB elimination commitment into their mandates, policies, and work programs, with the goal of promoting health-risk reduction behaviours and increasing demand for TB protection and care.
5. What is the aim of the PAAP-TB?
The PAAP-TB aims to address the nation’s TB epidemic by re-examining current programs and initiatives of TB-NCC member organizations. The high number of TB cases and the ineffectiveness of previous efforts prompted the use of a social determinant lens to address persistent diseases like TB. The incidence of TB in the Philippines exacerbates poverty and disparities experienced by the majority of the population.
6. What are the themes/sectoral clusters included in the PAAP-TB and what is their purpose?
The PAAP-TB serves as the focal point for addressing social determinants of health (SDH) and subgroups were formed to address specific variations of SDH. These subgroups facilitate collaboration among stakeholders and exchange of information and best practices to increase chances of concrete results.
Core members coordinate the work and lead each subgroup. The subgroups are tasked with fostering collaboration between the TB-NCC and stakeholders, exchanging information on their themes, and implementing their subsection in the PAAP.
social-protection2

The social protection sector will ensure vulnerable populations access to comprehensive, coordinated and essential healthcare services, and social protection packages, including those to combat TB.
1. Outcome:
Enhanced access and coordination in the provision of primary care services for beneficiaries
Key Interventions
A. Enroll beneficiaries i.e. 4Ps and AICS, to PCPNs to access Primary care services and COBP
B. Provide uninterrupted health services for beneficiaries
C. Provide EC sickness benefit for work-related TB claims
Output: Access of vulnerable population to TB/primary care services increased
1.1. No. 4Ps beneficiaries enrolled in Konsulta
1.2. % of residential clients in all facilities managed by DSWD enrolled in Konsulta (DSWD, PhilHealth)

Output: Availment of vulnerable population to TB/primary care services increased
1.3. Number of presumptive TB referred for further screening and case management

1.4. Number of TB sickness-related benefit claims related to work

2. Outcome:
Heightened awareness regarding access to and utilization of health services by the assigned population from accredited providers
Key Interventions
A. Conduct Awareness Activities i.e. FDS on TB, primary care services and COBP for beneficiaries
Output: Health education and training provided among/ advocates and family members

2.1.a. Number of 4Ps beneficiaries completed the FDS with TB module and COBP
2.1.b. Number of CRCFs onduvted activities on TB awareness
3. Outcome:
Improved indoor air quality of houses constructed for beneficiaries that have access to basic services
Key Interventions
A. Provide relocated families with adequately ventilated housing and basic health services
Output: Provide relocated families with adequately ventilated housing compliant with established housing standards and basic health services

3.1. No. of Relocatees oriented on available health facilities and essential health services near relocation site
3.2. No. of Relocatees assessed to health risk as conditionality for the resettlement area
3.3. No. of Relocatees referred to LGUs for access to basic primary care service
4. Outcome:
Increased multisectoral actions for TB prevention and control programs at national and regional levels
Key Interventions
A. Provide coordinated social protection packages i.e. health (PhilHealth), livelihood (DOLE), emergency shelter assistance (DHSUD) to vulnerable population/beneficiaries (DSWD) and 14 basic sectors (NAPC)
B. Organize convergence/facilitation platforms on TB & poverty reduction
C. Integrate TB-related programs/projects/activities into National/Local Poverty Reduction Plan (N/LPRPs)
Output: Increased coverage of social protection packages such as health (PhilHealth), livelihood (DOLE), emergency shelter assistance (DHSUD) and support to most vulnerable population (DSWD) and 14 basic sectors (NAPC)
4.1. Number of beneficiaries from the different social protection packages availing of Konsulta package

4.2. Number of agencies/LGUs with functional convergence platforms

4.3. Number of N/LPRPs with TB-related programs/projects/activities

education-public-information-and-community-engagement2

The Education, Public Information and Community Engagement sector will provide a gateway for comprehensive access to primary care in the learning institutions and lead the promotion of healthy habits among children, adolescents, young adults and the educational workforce.
1. Outcome:
Reduced incidence of smoking in young children and adolescents in learning institutions
Key Interventions
A. Expand Brief Tobacco Intervention (BTI) services in all public and private learning institutions
B. Offer BTI services to identified smokers including staff working in learning institutions
Output: BTI institutionalized in schools and HEIs
1.1. No. of trained personnel for BTI provision
1.2. Mapping and profiling of known smokers among learners and teaching and non-teaching personnel in the school system
1.3. No. of learners provided with BTI services
2. Outcome:
Expanded model or competency standards for community-based practice health workers
Key Interventions
A. Implement Micro-credential /Competency Standards program for community navigators
Output: Placement and integration of completers into the local system
2.1. Learning Institutions offering competency standards appropriate for community navigators
2.2. % Increase in deployed community-based trained navigators or workers
3. Outcome:
Adoption of healthy habits by population increased
Key Interventions
A. Advocate to Parent Association on Infectious Diseases such as TB, Malaria and the like with emphasis on the importance of regular check up and screening
B. Disseminate strategic information through available platforms i.e. Broadcast, Production/Ad Placement, Repackaging of available IEC materials
C. Establish Primary care service delivery in or near school settings
Output: Sustained promotion of healthy habits and behaviors through various platforms
3.1. Advocacy events/activities/trainings conducted to patient volunteers/advocates, parent associations/family members on infectious diseases
3.2.a No. of delivered/No. Requests for ads placement for TB and healthy habits
3.2.b Reach: Media mentions/impressions and/or page views/unique visitors
3.3. No. of schools/division clinics who are members of an accredited PCPN
labor-protection2

The Labor Protection Sector will guarantee employees continuous access to essential primary care services protecting workers’ right to good health and healthy workplace
1. Outcome:
Improved access to quality primary care services for workers
Key Interventions
A. Provide information to private establishments on how to access preventive and curative healthcare services
B. Conduct advocacy activities for NGAs and employee groups/cooperatives on primary care
Output: Sustained utilization of COBP services by workers, facilitated by their employers

1.1. % Inspected establishments with issued policies and programs on TB in the workplace
1.2. Issuance/policy for employee organizations of NGAs to have MOA with Konsulta-accredited facility for access to primary care
2. Outcome:
Establishment of a supportive and inclusive work environment for workers affected by TB
Key Interventions
A. Regular monitoring, training and sensitization of both workers and employers in private establishments
Output: Consistent and widespread observance of workplace policies, including provisions for the protection of workers from stigma and discrimination

2.1. No. of employers who accessed self-learning module
support-for-service-delivery2

The Support for Service Delivery sector will enable province and city-wide health systems with contracted primary care network to delivery comprehensive primary care across settings and accelerate TB elimination campaigns.
1. Outcome:
Enhanced health competencies and system capacities among SGLG awardees
Key Interventions
A. Measure and track LGU commitment to TB/primary care services
Output: Improved measurement and tracking of LGU commitment to TB/primary care service delivery through the updated SGLG metric for the health component that includes TB
1.1. Increase in the performance of existing indicators
– TB notification rate
– TB Treatment Success Rate (TSR)
2. Outcome:
Increased number of HRH complement to province and city-wide health systems
Key Interventions
A. Deploy community navigators (DILG)
Output: Enhanced health competencies & systems capacities
2.1. LGUs with deployed Community Navigators or Community navigators employed and deployed in LGUs
2.2. Number of CSOs and private providers accredited for training in LGUs
3. Outcome:
Functional integrated information system
Key Interventions
A. Develop integrated HIS tat will be used for surveillance
Output: Deployment of a fully-accepted proof-of-concept for the demonstration of an integrated health information system/HIS
3.1. Number of provinces/cities with interoperable HIS/EMR
4. Outcome:
Establishment of reliable and sustainable primary care services in special and/or fragile settings
Key Interventions
A. Include jails in referral networks
B. Accredit jail clinics as Primary Care Facilities (PCFs)
C. Expand APE/PEME requirement in Industries/Workplaces to Primary Care Services
Output: Expansion of health services for Persons Deprived of Liberty (PDLs), PDLs will be members of Philhealth, and Linked workplaces/schools with PCPNs
4.1. Number of jails with established referral network
4.2. Proportion of Philhealth-enrolled PDL members through DSWD mechanisms
4.3. Number of Konsulta-accredited clinics and/or Number of establishments/schools/workplaces provided with the process and access on nearby service delivery points
5. Outcome:
Increased accredited primary/health care provider networks
Key Interventions
A. Accredit primary/health care provider networks within P/CWHS
B. Incorporate Mandatory Notification in the licensing/ accreditation system
Output: Implementation of network-accredited province/city-wide health system (P/CWHS) and Streamlined reporting of TB notification
5.1. Number of accredited PCPNs with functional TB DOTS services
5.2. Percentage of facilities accredited by Philhealth using the updated certification/licensing and accreditation of networks
5.3. Number of New Technologies Approved
6. Outcome:
Zero stock-outs on essential medicines and commodities
Key Interventions
A. Support LGUs on efficient procurement, supply chain management, health planning, and investment
Output: % of LGUs implementing the (1) logistics and supply chain management training package; (2) augmentation of TB drugs
6.1. Number of provinces and cities provided with capacity development support on logistics and supply chain management

7. Outcome:
Increased engagement of LGUs in TB elimination advocacy campaigns
Key Interventions
A. Conduct information dissemination/advocacy campaigns in LGUs for TB elimination
Output: Information dissemination and stewardship activities in LGUs (ULAP, LPP)
7.1. Number of LGUs that conducted the info dissemination and stewardship activities on TB elimination i.e. smoking cessation, nutrition, support to housing relocation, etc.

8. Outcome:
Partnership with private sector (non-profit and profit) on TB Elimination expanded and sustained
Key Interventions
A. Issue guidelines for private sector participation in Konsulta package and PCPN
B. Advocate for participation to PCPN among the private providers
Output: More private konsulta providers providing TB services are members of or linked to PCPN
8.1. Number of advocacy meetings on Konsulta package and PCPN

Key Interventions
C. Provide incentive mechanisms to expand and make more effective the mandatory notification
Output: Mandatory notification of private providers expanded and institutionalized
8.2. Number of private providers notifying TB patients to NTP

Key Interventions
D. Advocate to more TB laboratories to join the Laboratory Consortium
E. Monitor performance
Output: Laboratory consortium expanded
8.3. Number of new laboratories who join the Consortium
8.4. Number of Rapid diagnostic tests (i.e. GeneXpert done)
Key Interventions
F. Pilot and document innovative solutions on the various TB care cascades
G. Advocate for adoption and expansion
Output: Innovative solutions for TB elimination among private providers developed and shared
8.5. Number of scalable innovations or standards on TB care cascade implemented and documented

Key Interventions
H. Conduct advocacy and educational activities on TB elimination
I. Develop and disseminate advocacy materials
Output: More private organizations join PhilCAT or similar network
8.6. Advocacy and educational activities conducted by private sector partners ie. World TB Day and Lung month celebrations